Ivermectin Exposure in Small Children Study Group
Ivermectin Exposure in Small Children Study Group
The Ivermectin Exposure in Small Children Study Group aims to assess safety profile of ivermectin exposure in children less than 15 kilograms
The Ivermectin Exposure in Small Children Study Group was formed Q2 2017, with call for any data from patients <15kg and treated with ivermectin. The call for data closed Q4 2019. The curation of the data and statistical analysis were completed in Q3 2020 and the manuscript, A systematic review and an individual patient data meta-analysis of ivermectin use in children weighing less than fifteen kilograms: Is it time to reconsider the current contraindication? was published in PLOS Neglected Tropical Diseases in March 2021.
Ivermectin is a widely used antiparasitic drug. It is approved for the treatment of onchocerciasis [1], lymphatic filariasis [2], strongyloidiasis [1] and scabies [3].
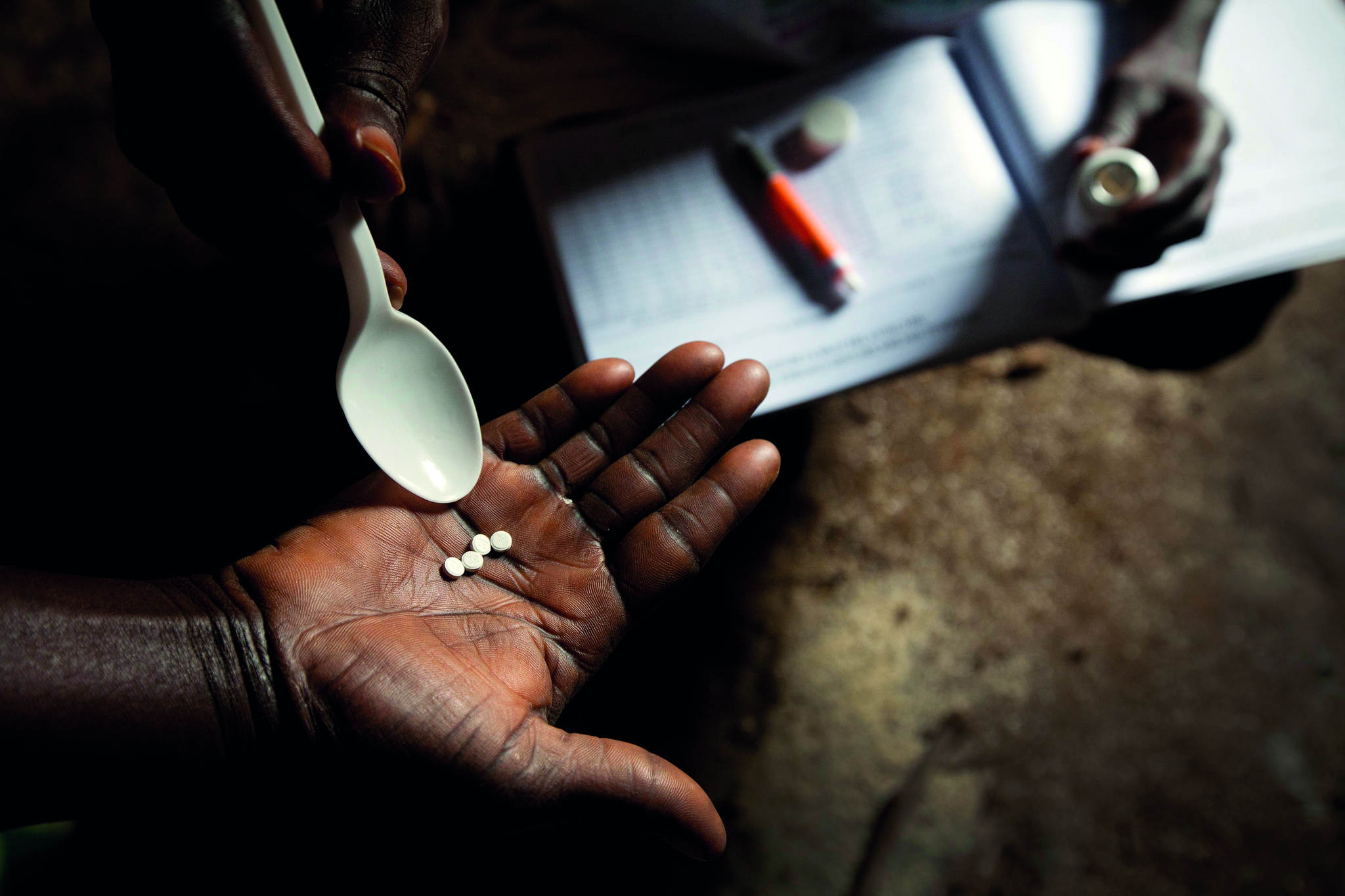
Billions of people have been treated with ivermectin during mass drug administrations (MDAs) for onchocerciasis and lymphatic filariasis. Recent evidence demonstrates that ivermectin MDAs can reduce scabies burden [4] and malaria parasite transmission [5].
When used in MDA for onchocerciasis, the population coverage achieved during drug distribution is a key factor for efficacy [6], a similar effect is expected for malaria [7] and scabies. The safety and effectiveness of ivermectin in children weighing less than 15 kg has not been established [1]. This means that children less than 15 kg are not treated during MDAs, since this group comprises roughly 20-30% of populations in malaria and scabies endemic areas. [4,5] this directly limits the proportion of people that can be treated during MDA, therefore challenging the MDA impact.
For malaria, ivermectin kills the Anopheles mosquito vector thereby reducing Plasmodium transmission [5]. Thus, having a portion of the human population not treated during ivermectin MDAs will reduce insecticide delivery to the blood feeding Anopheles populations, diminishing MDA value. In Africa, children younger than five years are frequently bitten by Anopheles mosquitos as evidenced by high rates of new malaria infections in this population. Thus, untreated children less than 15 kilograms serve as an important reservoir of Plasmodium and facilitate onwards transmission to mosquitoes.
For scabies, ivermectin kills the causative mite agent, Sarcoptes scabei. Children five years and under may have high prevalence of scabies compared to older age groups [8]. Since children less than 15 kg are not indicated for treatment with oral ivermectin due to a lack of safety evidence, topical creams such as permethrin or benzyl benzoate are used. However, topical creams are not always effective due to many reasons, including lack of compliance and adherence to application protocol when performed outside the clinical setting. Topical permethrin had lower scabies clearance rates than oral ivermectin in a recent MDA study in Fiji [4]. Non-ivermectin-treated children less than 15 kg could serve as a reservoir for scabies re-infection for the rest of the community during ivermectin MDAs, again reducing MDA impact.
In France, oral ivermectin can be used for scabies treatment in children less than 15 kg if primary topical permethrin and benzyl benzoate treatments fail [9]. Oral ivermectin has been used off-label in numerous clinical investigations and settings to treat children less than 15 kg for scabies, head lice, cutaneous larval migrans, strongyloidiasis, onchocerciasis, gnathostomiasis, and baylisascaris. To achieve these important goals, we aim to pool individual patient data of all known ivermectin exposures in children less than 15 kilograms, and assess any adverse events. The proposed work will provide evidence to inform the use of ivermectin in children less than 15 kilograms.
-
Compile all known ivermectin exposures in children less than 15 kilograms
- Assess adverse events following ivermectin exposure in children less than 15 kilograms
Any systematic reviews, clinical trials, observational studies, case-control studies, case series, case reports, and pharmacovigilance database entries that specifically report adverse outcomes after ivermectin exposure in children less than 15 kilograms will be included.
Minimum required data:
-
Weight
-
Adverse events associated with ivermectin
- Dosing regimen
-
Height and age
-
Gender
-
Ivermectin manufacturer and trade name
-
Country where ivermectin treatment occurred
-
Disease treated with ivermectin
- Concomitant medications and diseases treated
Once uploaded into the WWARN Data Repository, datasets will be standardised according to the WWARN Clinical Data Management and Statistical Analysis Plan (SAP). The SAP has been developed and is available for download.
The Study Group comprises investigators who contribute relevant datasets to the pooled analysis and invited technical experts. Datasets remain the property of the investigator. More details about sharing data with WWARN and how WWARN will use data are available on the WWARN website.
The Study Group collectively makes decisions with respect to including additional studies, data analysis and plans for publication, in line with the WWARN Publication Policy. Dr. Podjanee Jittamala and Kevin Kobylinski co-lead the Study Group, Kalynn Kennon leads data curation, and Caitlin Richmond is the Scientific Coordinator for the Study Group. All enquires to ivermectinSG@wwarn.org.
The Study Group is a collaboration between Mahidol University, AFRIMS, and WWARN.
1. Merck & Co.: Stromectol. FDA approved Package insert 2009 (accessed June 2015).
2. Ministere des affaires sociales de la sante et des droits des femmes: STROMECTOL 3 mg, comprimé - Résumé des caractéristiques du produit.
3. Merck & Co.: Stromectrol. TGA-Australia approved Package insert 2014 (accessed July 2016).
4. Romani L, Whitfeld MJ, Koroivueta J, Kama M, Wand H, Tikoduadua L, Tuicakau M, Koroi A, Andrews R, Kaldor JM, Steer AC: Mass drug administration for scabies control in a population with endemic disease. N Engl J Med. 2015, 373:2305-2313.
5. Alout H, Krajacich BJ, Meyers JI, Grubaugh ND, Brackney DE, Kobylinski KC, Diclaro JW II, Bolay FK, Fakoli LS, Diabaté A, Dabiré RK, Bougma RW, Foy BD. Evaluation of ivermectin mass drug administration for malaria transmission control across different West African environments. Malar J 2014, 13: e417.
6. Turner HC, Walker M, Churcher TS, Basanez MG: Modelling the impact of ivermectin on River Blindness and its burden of morbidity and mortality in African savannah: EpiOncho projections. Parasit Vectors 2014, 7:241.
7. Slater HC, Walker PG, Bousema T, Okell LC, Ghani AC: The potential impact of adding ivermectin to a mass treatment intervention to reduce malaria transmission: a modelling study. J Infect Dis 2014, 210:1972-1980
8. Karimkhani C, Colombara D, Drucker A, Norton S, Hay R, Engelman D, et al. The global burden of scabies: a cross-sectional analysis from the Global Burden of Disease Study 2015. Lancet Infect Diseases. 2017;17(12):1247-54.
9. Berthe-Aucejo A, Prot-Labarthe S, Pull L, Lorrot M, Touratier S, Trout H, Bourdon O, Dehen L, Bourrat E. Treatment of scabies and Ascabiol® supply disruption: What about the pediatric population?Archives de pédiatre 2014, 21: 670-675.

