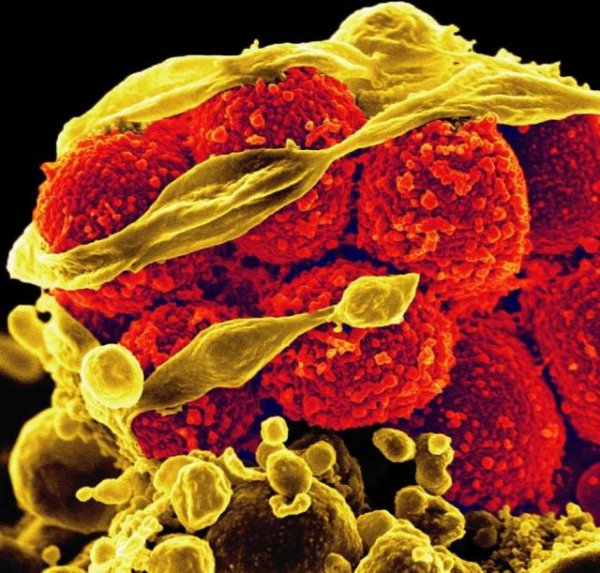
Understanding the drivers of antimicrobial resistance
The global fight against antimicrobial resistance could be under threat unless the evidence base for policies to control resistance is radically improved, according to a major new series of papers published in The Lancet.
According to one of the papers in the series, current guidelines are poorly understood, and policy makers have little reliable guidance to determine the best options to tackle the threat of antimicrobial resistance. The papers discuss how concerted action is needed to evaluate, develop and implement the best control measures to curb the emergence and spread of antimicrobial resistance (AMR).
Collectively, the series provides a comprehensive look at how AMR is currently being tackled, and the gaps in our current knowledge, and outlines the future priorities for researchers and policy makers. The papers also point out that access to antimicrobials and antibiotics can be challenging in many parts of the world. This puts many people – primarily infants and mothers – at risk of developing serious and life threatening symptoms from infectious diseases. In fact, more people die each year from lack of access to antimicrobials than from resistant bacteria.
The authors suggest that incentives for pharmaceutical companies to develop new antibiotics should be overhauled. “At the moment, the economic value of new antimicrobial drugs doesn’t materialise until the old drugs have failed, by which time it is too late,” says Professor John-Arne Røttingen, Executive Director of Environmental Health and Infectious Disease Control at the Norwegian Institute of Public Health and lead author of the studies. “We need to completely rethink the way that research into antimicrobials is funded, starting by decoupling innovation in drug development from sales. The funding of these drugs needs to be driven by public health needs, not by profit.”
Prof Philippe Guérin, director of WWARN, and co-author of one of the studies says: “The emergence of antimicrobial resistance is a natural evolutionary response to antimicrobial exposure, which requires further investigation and a coordinated approach. There are many complex and interlinking factors that are driving the prevalence of antimicrobial resistant organisms that are not yet fully understood.
“It is clear that we need to take urgent action to combat the threat to human health. In the case of malaria, the significant steps that have been taken to reduce the burden of the disease are threatened by resistance to existing antimalarial medicines. Artemisinin derivatives, the cornerstone of malaria treatment, are now under threat as resistance to this family of drugs has emerged and spread across Southeast Asia in less than a decade. If drug resistance spreads from Asia to the African sub-continent, or emerges in Africa independently as we’ve seen several times before, millions of lives will be at risk.”
The paper co-authored by Prof Guérin, 'Understanding the mechanisms and drivers of antimicrobial resistance', suggests that the problem of AMR is extremely complicated and there is no single solution that can tackle this colossal challenge. The transmission and emergence of resistance is affected by lack of access to sanitation – clean drinking water and closed sewage systems – variations in infection control practices, high population density and poor regulation of antimicrobial use in veterinary practice. The study states that to tackle the problem ‘several, synergistic, overlapping and complementing approaches will be needed, with a strong overarching shared goal to ensure and sustain access to effective antimicrobial therapies.’
“Our understanding of the mechanisms by which bacteria and other pathogens acquire resistance to drugs suggests that there will be no single solution to the global threat of antimicrobial resistance,” says Professor Alison Holmes, Director of the NIHR Health Protection Research Unit for Healthcare Associated Infection and Antimicrobial Resistance and Professor of Infectious Diseases at Imperial College, London, and lead author of one of the papers. “We need to tackle this problem synergistically, on multiple fronts, which will require an unprecedented level of international cooperation.”
The same can be said for the problem of antimalarial drug resistance. As the threat of antimalarial drug resistance grows, there is increasing pressure to sustain the efficacy of existing medicines and develop alternative treatments, as well as sustaining preventative measures such as bed nets. Cooperation among researchers, funders, pharmaceutical companies and governments across the world will be required to meet this challenge.
Publication details:
Holmes, A. H., et al. 'Understanding the mechanisms and drivers of antimicrobial resistance.' The Lancet. DOI:http://dx.doi.org/10.1016/S0140-6736(15)00473-0

