Assessing the need for a schistosomiasis treatment database
A database of individual participant-level information could benefit schistosomiasis clinical research and treatment policies, according to a study published today in PLOS Neglected Tropical Diseases.
The study was conducted by a group of researchers from the Centre for Tropical Medicine and Global Health at the University of Oxford, the Luxembourg Institute of Health and TDR.
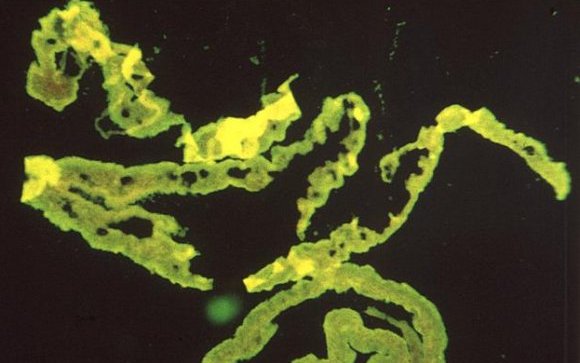
Schistosomiasis is a parasitic disease prevalent in tropical climates, especially sub-Saharan Africa. It is caused by schistosomes, parasitic worms that live in freshwater snails. Poor living conditions, overcrowding, and lack of sanitation, clean water and medical services increase the risk of schistosomiasis. Also known as bilharzia, the disease can cause anaemia and malnutrition, and after years of infection may also damage the liver, intestine, lungs, and bladder.
Schistosomiasis control and elimination mainly relies on preventive chemotherapy with praziquantel distributed to high-risk groups. Around 260 million treatments are administered yearly – so being able to assess and monitor how the drug works becomes very important.
Amélie Julé, a doctoral student at the Centre for Tropical Medicine and Global Health, and lead author of the paper said: “The review assessed the number of trials studying schistosomiasis medicines and looked at where these studies were conducted, in which populations, the drugs that were tested, and the dosage and methodologies used. Our aim was to determine the merit and scope of a common database of anti-schistosomal efficacy data.”
Guidelines for the treatment and control of schistosomiasis are supported by systematic reviews and meta-analyses. So far, these have been based on aggregated data, as published in scientific journals; this carries some limitations due to variations in how trials are designed, conducted, analysed and reported. Some of these limitations could be corrected by having access to individual participant-level data (IPD), which facilitates standardised analyses.
The study found that over 20,000 IPD on treatments for schistosomiasis could be gathered from 90 studies conducted in the past 15 years. The volume of data, and the differences in methodologies and reporting, indicate that there is scope for a schistosomiasis database to allow for standardised analyses.
Piero Olliaro, team leader for Intervention and Implementation Research at TDR, and co-author of the paper, said: “The importance of this finding rests in the ever-growing need for greater granularity in data to inform evidence-based policies, especially now that the use of praziquantel for preventive chemotherapy of schistosomiasis is expanding. Access to primary data from trials would make it possible to answer critical questions, such as differences in treatment efficacy in time and space and the optimum dose for young children. Much could be learnt about these treatments should it be possible to create a common database and standardise analysis.”
Data sharing maximises the utility of research and is promoted by the World Health Organization as a way of improving knowledge to inform policies. The schistosomiasis review drew upon data-sharing principles and processes developed by the Infectious Diseases Data Observatory and The Global Health Network.
Amélie Julé is conducting her doctoral research at the Centre for Tropical Medicine and Global Health at the University of Oxford. She is mainly investigating the data management practices of teams working in resource-limited institutions and based in low and middle income countries (LMICs). Understanding the needs and accordingly strengthening local capacity for clinical research and data management is crucial to generate more, better quality data on neglected tropical diseases like schistosomiasis, as well as to facilitate future data-sharing and thus enable meaningful secondary analyses of data.
Publication details:
Julé AM, Vaillant M, Lang TA, Guérin PJ, Olliaro PL (2016) The Schistosomiasis Clinical Trials Landscape: A Systematic Review of Antischistosomal Treatment Efficacy Studies and a Case for Sharing Individual Participant-Level Data (IPD). PLoS Negl Trop Dis 10(6): e0004784. doi: 10.1371/journal.pntd.0004784

