The DEG-EG Project: Safety of medicinal syrups for children
The DEG-EG Project: Safety of medicinal syrups for children
There have been multiple outbreaks of poisoning due to diethylene glycol (DEG) and ethylene glycol (EG) in paediatric medicine syrups. They have killed many hundreds of children worldwide. Reference tests to detect these are expensive, complicated and only available in sophisticated laboratories. We are evaluating innovative techniques to screen for DEG & EG in raw ingredients and syrups in supply chains to explore methods for medicine inspectors to be empowered to screen and select samples for reference assays.
Diethylene glycol (DEG) and ethylene glycol (EG) are used in the manufacture of products such as antifreeze and glues, but should never be incorporated in human pharmaceuticals as they are toxic. However, since the first outbreak in the USA in 1937 there have been multiple reports of their presence in paediatric cough and paracetamol syrups. For example, since 2022 there have been reports from The Gambia, Uzbekistan, Indonesia, Pakistan, Cameroon, Nigeria, Lao PDR, the Maldives and the Marshall Islands & Micronesia.
DEG & EG cause multiorgan failure, especially acute renal failure and neurological dysfunction, and have resulted in hundreds of deaths, especially of children. The presence of DEG & EG has been caused by errors in manufacturing processes and substitution of the recommended pharmaceutical grade glycol excipients, glycerine, and propylene glycol (PG), that are used in good quality cough and paracetamol syrups.
There are allegations in some incidents pointing to deliberate mislabeling of the less expensive toxic glycols as pharmaceutical grade bulk excipients, resulting, when not checked by pharmaceutical manufacturers, in the finished product being contaminated with lethal levels of toxins.
The usual reference assay for detecting DEG & EG is gas chromatography with flame isonisation detection (GC-FID) but this is expensive, complicated and not commonly available in low- and middle-income countries (LMICs) where contaminated syrups are mostly reported. There are currently no widely available, inexpensive, easy to use or portable devices for inspectors to screen for DEG & EG.
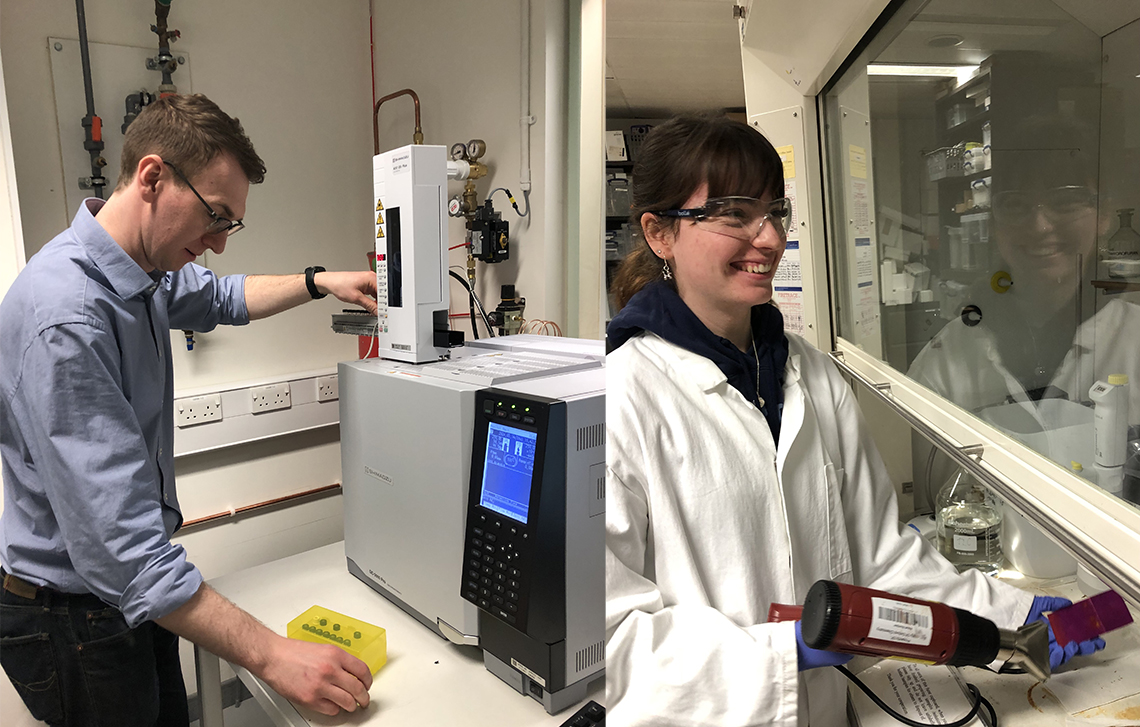
Building on experience and knowldege gained during the Vaccine Identity Evaluation (VIE) Collaboration, to investigate affordable screening devices for detecting substandard and falsified vaccines, we are evaluating devices to detect DEG-EG contaminated paediatric syrups. We are not expecting these to replace current reference assays, but to have more widely available, simpler and affordable techniques to allow inspectors to screen more rapidly at various points of supply chains for suspected samples that need reference assays. This links up the Medicines Quality Research Group (PI - Prof Paul Newton, within the Nuffield Department of Medicine), the Department of Biochemistry (PI Prof. Nicole Zitzmann), the Department of Chemistry (PI Prof. James McCullagh), the Rutherford Appleton Laboratory (RAL, PI Prof Pavel Matousek) of UKRI and the University of East London (Prof Hamid Merchant), with multiple international collaborators, including WHO, pharmacopeias, toxicologists, medicine regulators, reference laboratories and device manufacturers.
We are investigating, in comparison to GC-FID, thin-layer chromatography (TLC), Matrix-assisted laser desorption/ionization-time-of-flight mass spectrometry (MALDI-TOF), atmospheric solids analysis probe-mass spectrometry (ASAP-MS), handheld spatially-offset Raman spectroscopy (SORS), and diverse lower cost devices and techniques.
We are very grateful for the funding for this work from the Bill & Melinda Gates Foundation and Medicine Quality Research Group support from the Wellcome Trust


